Another Pandemic Looming? The Mpox Saga
Aims:
Just like every other article you have read on the internet, there are aims to this article.
In this article, we seek to help you understand mpox by providing a comprehensive overview of the disease, highlighting its symptoms, transmission, and the significance of this current outbreak.
This article also seeks to raise awareness and promote informed discussions about the prevention and treatment of mpox while emphasizing the role the community plays in combating this viral disease.
Given:
mpox, monkeypox, global, viral outbreak, public health, transmission, symptoms, awareness, prevention
Method:
An essay
Principle:
Mpox, a viral disease caused by the mpox virus, has recently re-emerged as a significant public health concern. Originally identified in the late 1950s, mpox has primarily affected regions in Africa but is now posing a threat globally. Understanding mpox is crucial, as its symptoms can mimic other illnesses, and its transmission routes highlight the need for heightened awareness and preventive measures. As cases continue to rise, it is essential for individuals and communities to be informed about the disease and its implications.
Procedure:
An Overview of Mpox
Viral diseases have been one of the major global health crises that the world has been battling nonstop over the past decade. From Lassa fever to Ebola to COVID-19, humanity has lost countless souls, soldiers and civilians alike, in this seemingly unending battle with these “environmental” microbes. We have barely recovered from the devastation of the last viral outbreak, COVID-19, and already it looks like we are on the verge of another pandemic.
From your dailies, you may have caught wind of several reports on the outbreak of mpox, and just like some people, you might have asked the biggest question: What exactly is it?
A bit of history: the genesis…
Mpox traces its history as far back as the 1950s when it was called monkeypox.
Why monkeypox?
As with many nomenclatures in science, this disease got its previous name in a pretty straightforward manner: from the first group of animals, the disease was isolated and identified.
Colonies of monkeys kept for research in 1958.
However…
…in 2022, monkeypox was renamed to Mpox.
This name change was a decision made by the World Health Organization for several reasons ranging from:
the desire to reduce stigmatization associated with the name monkeypox (people naturally assumed that anyone with monkeypox had an association with monkeys),
clarify transmission routes especially given that many of its recent cases were through human-to-human with little to no contact with animals,
reduce the disease's association with just Africa and;
abide with scientific naming conventions of using combinations of letters or numbers for unique disease names.
Monkeypox, now Mpox, what then is it?
A definition
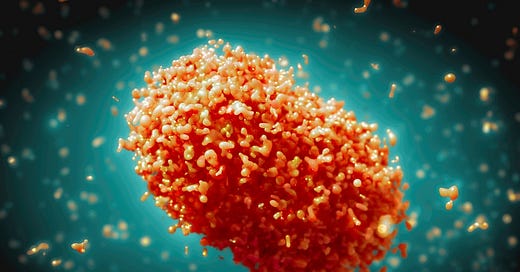
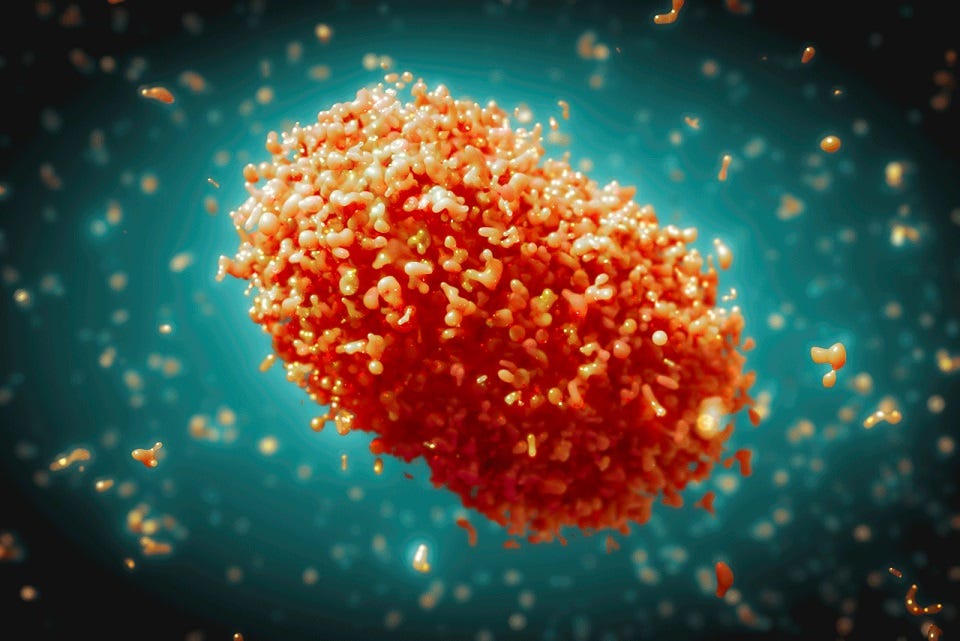
Mpox is a viral disease caused by the Mpox virus, belonging to the same family as smallpox and cowpox: the Orthopoxvirus genus. Members of this virus family typically cause diseases characterized by outbreaks of rashes on the skin, and by implication, Mpox also presents with rashes on the skin as well as other symptoms such as fever, swollen lymph nodes, and joint pain.
…an outbreak ensues and continues
12 years after this disease's initial identification, in 1970, the first human case was recorded in the Democratic Republic of Congo (DRC).
Within the 1970s and 1980s, after this first human case of Mpox, more human cases were recorded, albeit infrequently and confined to the Central and Western regions of Africa, especially in rural communities with a lot of contact with wildlife. As the 1980s gave way to the 1990s, outbreaks started stepping out of the confines of these localized regions. Cases were recorded in regions outside the endemic regions, which began to draw the eyes of global health bodies.
However, it wasn’t until the first case was recorded outside the shores of Africa in 2003 that the world finally took note of the potential Mpox had for moving from an endemic disease to a possible pandemic. This recorded case was in the United States of America, with over 70 confirmed cases.
The DRC continued to record occurrences of Mpox; however, when it reached an all-time high in 2017, the international community had to step in to help with surveillance and response strategies.
While the world battled with COVID-19 from 2019 until 2021, Mpox was relatively silent. Then 2022 set in, and Mpox raised its ugly head again, this time crossing serious boundary lines and affecting countries that aren’t even remotely connected to the traditional endemic regions of the disease, indicating a shift in the virus’s transmission patterns.
It became more than a disease endemic to Central and Western Africa.
Where we are right now
Mpox is a zoonotic disease, which means that it can be passed from animals to humans on contact. Whereas before, this disease was confined to its endemic regions, with the recent development of its incidence in new geographical locations, strategies have been developed to prevent further spread. Among these strategies are a combination of surveillance, vaccination, and public health education (like this article seeks to provide you with).
In monitoring, managing, and mitigating the impact of the Mpox outbreak, global health authorities like the World Health Organization (WHO) and the Center for Disease Control (CDC) play frontline roles.
Identification of Mpox: Signs and Symptoms
The signs and symptoms of Mpox are not as distinct as you might like to think. As already mentioned, it may present with signs and symptoms similar to those of other diseases within its family and even of other common ailments. This means that someone you know may have Mpox, and you could easily point to another disease condition.
Because globally, there have been several reports on the increasing number of recorded cases across different countries, global health organizations, and indeed, we at MedLabConvo deem it fit to make you understand that it is VERY important that you do not dismiss any of these signs and symptoms:
High and sudden fever, often one of the first signs
Chills, which usually accompany the fever
Intense and persisting headache
Generalized muscle pain
Fatigue and a general feeling of malaise
Back pain
Swollen lymph nodes: Lymph nodes are small organs found scattered around the body at different locations that help fight infections. Of them, the ones found at the neck region are the most popularly known. A swelling in these lymph nodes should not be dismissed.
Rashes: The rashes start as flat, red bumps, which can be painful. These bumps turn into blisters, which fill with pus. Then, they crust over and fall off. The entire process lasts about 2-4 weeks, and the rashes cover everywhere from head to toe.
It is worthwhile to note that not everyone with Mpox will develop all of these symptoms. Symptoms could vary from person to person and in severity as well. Some people with Mpox will develop rashes, while others won’t.
Some might have few rashes in particular regions, while others may experience widespread rashes. Therefore, it is entirely possible to have Mpox and not know. Hence the importance of conscious awareness. Early detection is important to curb the spread of the virus.
Transmission Dynamics: How Mpox Spreads
Mpox spreads when one comes into contact with an animal or a person infected with the virus.
Person-to-person transmission occurs when one comes into contact with the sores, scabs, respiratory droplets, or oral fluids of an infected person through close contact.
Animal-to-person transmission occurs through broken skin from bites or scratches from an infected animal. Infection can also come through direct contact with bodily fluids or pox lesions in an infected animal.
The infected material route of transmission. Here, close contact with contaminated bedding, clothing, or other linens used by an infected animal or person could lead to an infection.
Taking action: Protecting yourself and those around you
Mpox is an easily transmissible disease, and just like other infections preceding it, there are ways you can protect yourself against catching it.
Practicing personal hygiene like regular handwashing with soap and running water; being mindful of unconscious habits like touching the face
Social distancing, including the use of face masks in high-risk areas or when in contact with infected individuals
Getting vaccinated. There is currently no vaccine specifically for the mpox virus, however, the vaccines available for smallpox also provide immunity against the mpox disease.
Go for regular checkups and be very vigilant about symptoms like swollen lymph nodes, fever, and rashes, no matter how small or scanty. Do this for yourself and the people around you.
Community Impact: Your role as a member of the community
Your role as a member of a community, small or big, is not to be a gossip. When it comes to disease, outcomes often largely depend on the efforts of community members to combat that disease.
As a member of that community, what should you do about Mpox?
One, have open discussions about it. Two, do not peddle rumors or stereotypes; rumors and stereotypes always cause more harm than good. Whatever information you pass along in these discussions should be accurate and not intended to incite panic. Three, work towards dispelling the stigmatization of those with Mpox. These people need your support through the period of their infection, and it will do them plenty of good to see that people care about their welfare. Lastly, do all you can to prevent an outbreak of the disease.
Comments:
In conclusion, Mpox represents a pressing public health challenge that requires collective awareness and action. By understanding the nature of the disease, its symptoms, and how it spreads, we can better equip ourselves to combat this outbreak. It is crucial for communities to engage in open discussions about mpox, dispel stigma, and promote preventive measures. As we navigate this public health crisis, let us remember that knowledge is our most powerful tool.
Recommendations:
Stay informed through reliable sources about mpox and public health guidelines.
Encourage open conversations about mpox to reduce stigma and promote understanding.
Advocate for community health initiatives that focus on prevention and support for those affected.