AIM:
The mass migration of professionals from Nigeria, christened ‘Japa’, is a popular trend driven by socio-economic and systemic factors. This article aims to discuss the trend within the healthcare context, examine the motivations behind it, the role of governing councils, and the implications of national policies on the future of Nigeria’s healthcare sector.
OBJECTIVES:
To examine the driving factors behind the Japa trend among Nigeria’s health workforce, particularly systemic issues like national policies, governing councils, and working conditions.
To assess the impact of the health workforce exodus on Nigeria’s healthcare system and its long-term implications for the sector.
To encourage conversations around potential solutions that could address the root causes of health workforce migration in Nigeria.
GIVEN:
Japa, health workforce migration, governing councils, working conditions, and the National Policy on Health Workforce Migration.
METHOD:
Creative / Expository essay
PRINCIPLE:
‘Japa’ is a Nigerian slang term that symbolises both hope and frustration. It comes from the Yoruba language, where it means "to flee" or "to dash." The slang was originally used in casual settings to describe someone trying to escape a tough or unpleasant situation, like a Saturday night party that suddenly turns sour. In such a scenario, a person might say to another: “Ah! Make we find way japa from here o,” expressing an urgent need to escape imminent danger.
Over time, the usage of the word evolved beyond a simplistic, casual meaning to describe emigration. In a 2018 song titled Japa, Nigerian artist Naira Marley repeatedly chants the slang in verses that portray a readiness to leave the country for destinations such as Canada or Chicago. Although this nuanced meaning cannot be traced to a single origin, it has become widely adopted on social media, making ‘japa’ one of the most popular terms for emigration, especially among Nigerian youths seeking better opportunities abroad.
Like twin peas in a pod, however, the buzzword regularly features alongside another term: brain drain. This is because, in recent years, the phenomenon has included a significant number of skilled professionals, including those in the healthcare sector. Beyond being a fleeting dream, japa has become a significant factor in the decision-making process for many young Nigerians when choosing a career path.
In a country where job opportunities are limited, economic instability is rampant, and prospects for advancement are often uncertain, planning for one's future must be strategic. For many young professionals, this means prioritising fields or engagements that offer higher chances of international relocation. Japa seems to have become the ultimate Nigerian dream. But what does this mean for the healthcare sector, whose workers migrate en masse every year? What is the genesis of this exodus, and how can the lamentations of the health workforce in Nigeria be addressed?
PROCEDURE:
Health workforce migration describes the movement of healthcare professionals - medical laboratory scientists, doctors, nurses, pharmacists and other allied health workers - from one country to another, often in search of better working conditions, career growth opportunities, or improved quality of life. Globally, this trend has been influenced by disparities in healthcare systems, economic conditions, and policies. When these professionals move from their country of origin to another, the movement is more precisely referred to as emigration. In Nigeria, emigration has reached alarming levels, as thousands of healthcare workers leave annually for developed countries like the United Kingdom, Canada, Switzerland and the United States. As the 2025 work and graduate school cycle begins, yet another significant wave of migration is expected.
Prof. Tosan Erhabor, Registrar of the Medical Laboratory Science Council of Nigeria (MLSCN), revealed that 10,697 medical laboratory scientists have emigrated, including 4,504 in 2023 alone. Earlier in 2024, Nigeria's Health Minister Muhammad Ali Pate also noted that between 15,000 and 16,000 doctors have departed in the past five years. The doctor–patient ratio in Nigeria is now an alarming 1:9,083 ratio, which is far below the recommended 1:600 ratio. Between 2002 and 2021, a total of 60,729 Nigerian nurses migrated to the United Kingdom. Skilled professionals from other health and health-related fields have not been spared by the emigration ‘flu’ either.
This sobering reality goes beyond mere statistics; behind the numbers are individuals striving for a chance at survival. The post-COVID global labour shortage in healthcare has made Nigerian professionals even more attractive to foreign employers, further fueling the ‘japa’ trend in the sector. What are the other driving factors behind this trend?
LAMENTATIONS OF A STIFLED WORKFORCE
INFRASTRUCTURE DEFICIT IN THE HEALTH SECTOR
In bustling cities like Lagos, life moves at a rapid pace. Healthcare workers are stretched as thin as sliced ugu leaves - mentally, physically, and emotionally.
On one such day, Dr. Vwaere Diaso closed her shift, worn out and drained. As soon as she got to her room on the 9th floor of the hospital, she did what almost anyone in her shoes would - she ordered food. She must have felt some relief when she received a call saying her meal had arrived.
With the excitement of someone about to be nourished after a long day, she left her room and walked into an elevator. Unfortunately, she did not walk out. The elevator had suddenly jolted. Its cables snapped, and the machine lost control. Life quickly became a blur as the elevator dropped, crashing to the ground. In there, trapped for 60 long minutes, the young doctor cried, hoped and screamed for help. By the time help arrived around 7:50 pm, she was barely clinging to life and by 8:59 pm, she was pronounced DEAD.
Late Dr. Vwaere Diaso (Image from X)
Dr. Vwaere Diaso, a graduate of Babcock University, was nearing the end of her mandatory one-year internship at the General Hospital, Odan, Lagos Island when this tragic accident occurred. All it took to end the dreams of that young doctor was two hours, neglect and a faulty system. The elevator at the hospital had been faulty for over three years, with numerous complaints lodged by both staff and patients. Yet, no meaningful action was taken. Dr. Diaso’s accident is a heartbreaking reminder of the infrastructural flaws that plague Nigeria’s healthcare system, where lives are too often left vulnerable to unchecked decay.
Infrastructure deficits in Nigeria’s healthcare system are widespread and deeply concerning. Upon graduation, many medical laboratory science professionals eagerly look forward to their one-year mandatory internship. For some, securing a placement takes only a few weeks; for others, it drags on for months, and for a few, it feels like an eternity. Yet, once they begin, the excitement often fades as they confront the harsh realities of Nigeria’s healthcare system.
Studies highlight numerous cases of dilapidated hospital buildings, malfunctioning equipment, and a lack of basic amenities like electricity and water. For instance, a 2021 survey by BudgIT revealed that over 80 per cent of Primary Healthcare Centers (PHCs) lacked essential infrastructure such as functional toilets and clean water supply. In tertiary hospitals, critical facilities like laboratories, diagnostic machines, and other essential equipment are often nonfunctional due to poor maintenance. These gaps in infrastructure not only undermine the quality of healthcare but also compromise the safety of everyone who relies on these facilities. This, in turn, correlates with the brain drain effect.
AN EVIL DUO: POOR WORKING CONDITIONS AND REMUNERATION
One of the most pressing challenges facing Nigeria’s healthcare system is the issue of poor funding and remuneration, which significantly motivate workers to ‘japa’. Many healthcare professionals, including medical laboratory scientists, nurses, and doctors, earn salaries that are not only low but also inconsistent. Delayed payments are also common in government-run hospitals. Despite years spent in rigorous training, these professionals often find themselves unable to either support their families adequately or afford the basic necessities of life. On a professional platform like LinkedIn, it is not uncommon to meet a healthcare professional with four other ‘side hustles’/ interests.
Medical Laboratory Scientist| Virtual Assistant| Writer | Baker | Pastor. #BringAllDeals
The low salaries, coupled with the rising cost of living and increasing inflationary pressure in Nigeria create a good recipe for frustration but one ingredient is missing - poor working conditions.
Mix the ingredients,
Stir
and Add Tears to Taste
For medical laboratory scientists, in particular, laboratories are frequently ill-equipped, with outdated or even unavailable diagnostic machines. As a result, some scientists must rely on manual methods for testing, which are slow, error-prone, and less effective. Many facilities lack essential reagents and materials, making even basic tests impossible to carry out. Overcrowded workspaces, inadequate ventilation, and poor waste disposal systems expose these professionals to biohazards, increasing the risk of infections and injuries. These conditions compromise the safety of health workers and limit their ability to deliver accurate results.
The situation becomes even more dire in understaffed facilities, where each healthcare worker feels the strain as if their energy and spirit are being slowly drained away. These challenges have forced many healthcare workers to seek opportunities abroad, where they believe their skills will be more valued and rewarded.
INSECURITY, YET ANOTHER CATALYST
Everyday life in Nigeria appears to be overshadowed by the constant threat of violence. Between May 2023 and April 2024, Nigerians paid ₦2.23 trillion in ransoms to kidnappers, according to the National Bureau of Statistics (NBS). The NBS report recorded 51.89 million crimes nationwide, with the North-West leading at 14.4 million cases, the North-Central at 8.8 million, and the South-East reporting the least with 6.18 million cases.
The survey also showed that 9.6 percent of Nigerians perceived themselves to be at risk of falling victim to crime within the next 12 months. Just like other Nigerians, health workers often face insecurity both in and out of the workplace. Healthcare professionals working in or operating within conflict-prone areas may either fall victim to violence or be targeted.
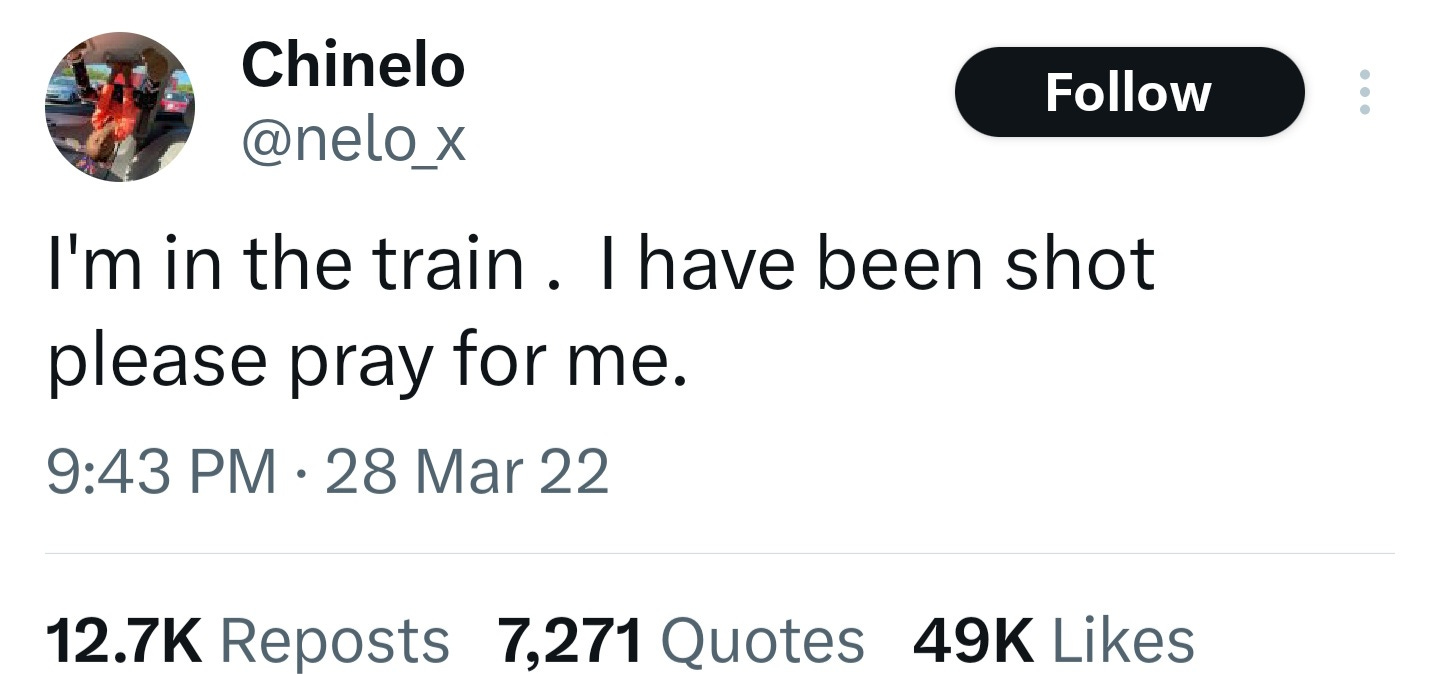
Perhaps you remember Chinelo Megafu, a Nigerian dental surgeon, who was tragically shot and killed during a terrorist attack on the Abuja-Kaduna train on March 28, 2022. Or the 20 medical students and a doctor who were kidnapped in Benue State while attending a convention. Or the consultant gynecologist who was abducted from his home in Zamfara State in October 2024. From constant threats of violence to kidnappings and insurgent attacks on communities, such instances abound.
Given these realities, the mass exodus of healthcare workers is hardly surprising. Their decision is not about a lack of patriotism but about seeking dignity, security, and a chance to live fulfilling lives.
THE PLACE OF POLICIES AND REGULATORY COUNCILS
Governing councils, such as the Medical Laboratory Science Council of Nigeria (MLSCN), the Medical and Dental Council of Nigeria (MDCN), Medical Rehabilitation Therapist Board (MRTB), and Nursing and Midwifery Council of Nigeria (NMCN) are major players in the healthcare sector. Unfortunately though, inefficiencies within these regulatory bodies often worsen the migration crisis.
From undergraduate studies through indexing, internship, and work life, many healthcare professionals feel unsupported by their councils. Some have pointed out that these councils only seem attentive during license renewal periods, with minimal effort made to improve working conditions, enhance capacity building, or even just address the persistent concerns of their members. This sense of neglect have pushed many to seek opportunities in countries where regulatory systems are perceived as more efficient and supportive.
The MLSCN has yet to implement direct restrictions on migration, unlike the NMCN, which recently introduced a policy requiring nurses to complete two years of post-qualification experience in Nigeria before seeking overseas opportunities. This policy triggered public outrage for failing to address the root causes of migration, such as low pay and poor working conditions.
Rather than impose restrictions, councils like the MLSCN should focus on solutions that directly benefit professionals. Improving working conditions is an important first step. This could involve advocating for competitive salaries, better welfare packages, and the provision of modern equipment and facilities. When professionals have access to the tools and resources they need to perform effectively, they are more likely to feel valued and motivated to stay.
MedLabConvo's LabCast has a podcast episode on MLS practice from a diasporic perspective.
A QUANTITY AND QUALITY DILEMMA
An issue MLSCN needs to consciously address is the oversupply of medical laboratory scientists in Nigeria. Universities admit large numbers of students annually, often far exceeding the council's indexing quota. This places untold pressure on students, department heads as well as the council itself. With the uncontrolled population and limited opportunities, many are left with no choice than to join the japa trend. The net result? A paradox where the nation trains more scientists than it can absorb, yet faces a critical skills gap as many leave to stand a chance at a fulfilling career!
Adding to this challenge is the proliferation of substandard laboratories. The MLSCN's lab registration policies are designed to regulate and maintain the quality of medical laboratories in Nigeria. Despite this, "mushroom" labs continue to sprout and undermine professional standards and public trust.
Our role in healthcare delivery is so critical that we cannot afford to have any quality issues.
Tightening regulations and ensuring strict enforcement will create an environment where skilled scientists can thrive locally. Whether through licensing fees or other charges, the overemphasis on monetary gain by councils is dangerous.
THE NATIONAL POLICY ON HEALTH WORKFORCE MIGRATION
It goes without saying that until the underlying systemic issues are addressed, the mass migration of health workers will remain an inevitable outcome of a broken system. In August 2024, Nigeria introduced the National Policy on Health Workforce Migration to address the growing brain drain in the healthcare sector. Its objectives include:
Retaining healthcare professionals by improving remuneration, health insurance, job conditions.
Strengthening the healthcare system by using managed migration to enhance capacity and efficiency.
Establishing agreements with destination countries to manage brain drain.
Creating opportunities for Nigerian healthcare professionals abroad to return and contribute to the health system
While its intentions are commendable, the policy has several gaps that makes it, well, idealistic. For one, many of its provisions are theoretical, with little evidence of practical impact. The policy also fails to address the unique needs of professionals in rural or underserved areas. It preaches high-sounding solutions like telemedicine whereas numerous medical facilities still struggle with efficiently managing manual processes. The policy seems disconnected from the realities obtainable in Nigeria’s healthcare system.
RECOMMENDATIONS:
Introduce competitive pay structures for healthcare workers, reviewed regularly to match inflation and global standards.
Invest in upgrading hospital infrastructure and equipping facilities with modern diagnostic and treatment tools.
Strengthen oversight measures to ensure healthcare funds are used transparently and effectively.
Collaborate with unions to identify grievances before developing policies.
Simplify employment processes and eliminate bottlenecks in recruitment for government hospitals.
Regulatory councils need to actively monitor member welfare, address grievances promptly, and advocate for improved working conditions.
It falls on the various tiers of government to improve systemic challenges like rising inflation levels, hardship and insecurity.
COMMENT :
The continued migration of healthcare professionals has severe repercussions for Nigeria’s healthcare system. In the short term, staff shortages can hinder access to services, especially in rural areas. Additionally, overworked professionals are more prone to errors that compromise patient care. In the long run, losing skilled workers weakens the health system and limits its capacity to respond to health emergencies like the recent MPOX outbreak. This might demand a reliance on expatriate workers or foreign-trained personnel. Where this option is unavailable - and it hardly is- working conditions become even more back-breaking.
To address these challenges, the government must reassess its workforce policies and align them with the realities of healthcare migration. Improving working conditions, investing in infrastructure, and creating clear career development pathways are non-negotiable steps. These measures can improve job satisfaction and help to reduce the outflow of skilled healthcare professionals from Nigeria.











This is an amazing read! Spoke my mind and even more
This is epic 👏
I had a really good read
This article highlighted lots of the concerns faced currently by professional bodies and workable solutions too.
I highly recommend!